Intermittent fasting or calorie restriction: which of the two is more effective at lowering blood sugar levels?
Intermittent fasting as most of you already know, is an eating plan that switches between fasting and eating on a regular schedule. It doesn’t specify which foods you should eat but rather when you should eat them. It is based on the idea that abstaining from eating for certain periods of time can have health benefits beyond weight loss, such as improved brain and heart health, increased resistance to stress, reduced inflammation, lowered blood sugar and insulin levels, improved insulin resistance, and reduced risk of type 2 diabetes and heart disease.
There are several different ways of doing intermittent fasting, such as:
The 16/8 method: You skip breakfast or dinner and restrict your daily eating period to 8 hours, such as 1–9 p.m. and you fast for 16 hours in between (including the night period when you are sleeping).
Eat-Stop-Eat: You fast for 24 hours, once or twice a week, for example by not eating from dinner one day until dinner the next day.
The 5:2 diet: You consume only 500–600 calories on two nonconsecutive days of the week, but eat normally the other 5 days.
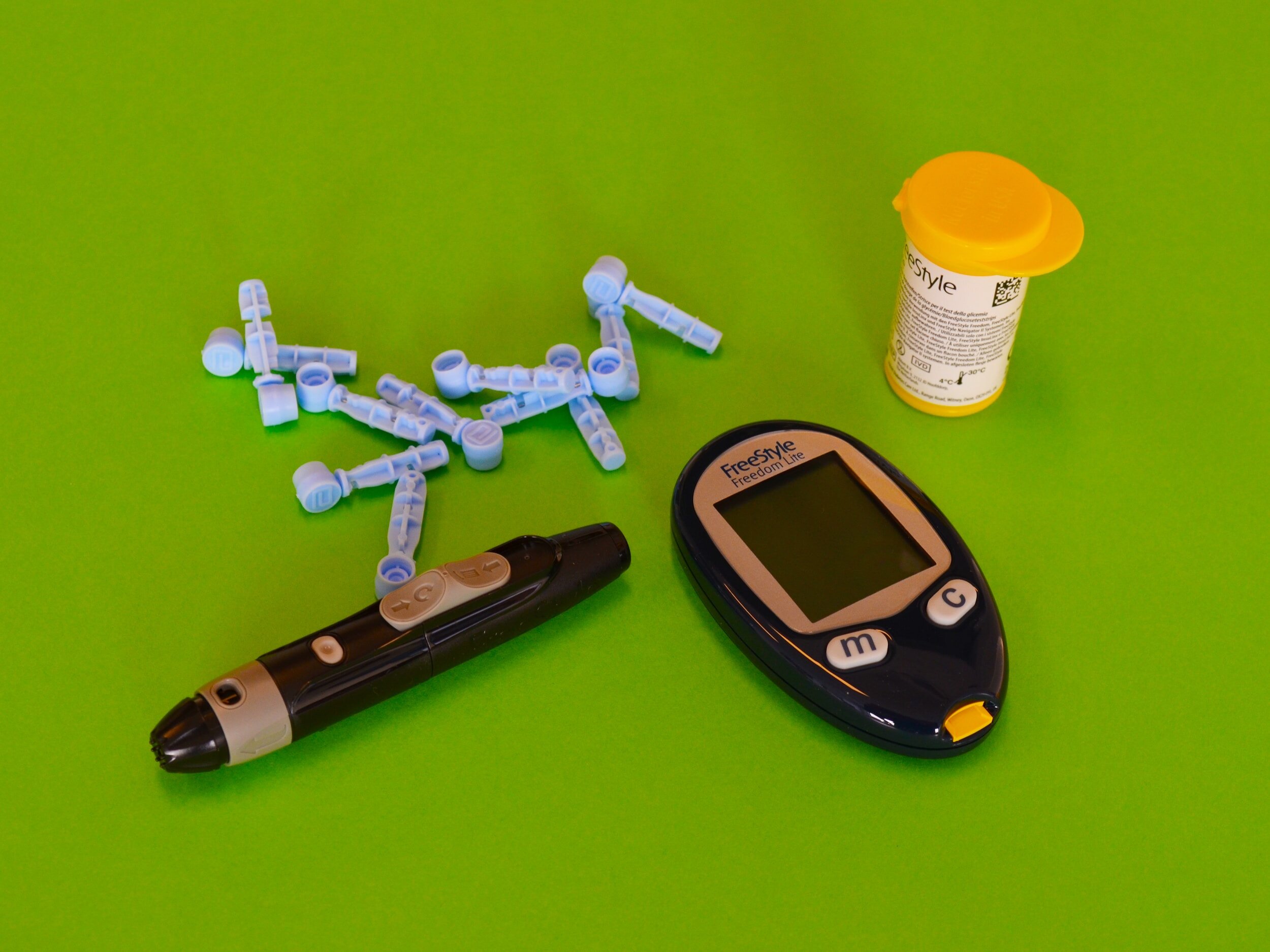
However, please note that intermittent fasting may not be suitable for everyone, especially people with diabetes, low blood pressure, or eating disorders. If you have any medical conditions or take any medications, you should consult your doctor before starting intermittent fasting. Especially people with diabetes who take medication to lower their blood sugar should consult their doctor first and monitor their blood sugar closely prior to trying intermittent fasting.
How does this work?
Intermittent fasting works by basically getting insulin levels low enough so your body burns stored fat for energy instead of sugar. When your body breaks down the food you eat, it ends up as molecules in your bloodstream. Insulin helps these molecules enter your cells where they can be used for energy or stored for later use. When you fast, your insulin levels drop and your cells start using fat as fuel.
Intermittent fasting works by prolonging the period when your body has burned through the calories consumed during your last meal and begins burning fat. It may also affect your hormones, cells, and genes in ways that promote longevity and disease prevention.
Some studies report that intermittent fasting can improve blood sugar even without weight loss, while others suggest that weight loss is the main factor for blood glucose balance. The effects of intermittent fasting on blood sugar may depend on changes in signaling pathways, metabolic rhythm, and ketones, but they may not last if the fasting protocol is discontinued and it may take 2-4 weeks of intermittent fasting to see significant improvement on blood sugar.
Differences Between Intermittent Fasting and Calorie Restriction
Intermittent fasting involves eating at certain times and eating nothing during other times of the day. This can indeed help reduce blood sugar levels, lose weight, and improve overall health as many studies have shown over the years.
Calorie restriction on the other hand involves reducing the amount of calories consumed each day. This can obviously help with weight loss and improved health, but it can also be difficult to track sustainably.
The link between type 2 diabetes (T2D), intermittent fasting (IF) and calorie restriction
Type 2 diabetes is a chronic condition that affects how the body uses glucose as an energy source, which over time can damage nerves and blood vessels. Blood sugar levels are high because the body does not produce enough insulin or cannot use insulin properly. More than 400 million people worldwide suffer from T2D.
One study compared the effects of IF and calorie restriction on blood sugar levels in people with T2D. Participants followed a 6-month diet in which they either practiced IF or followed calorie restriction. Both groups lost weight and saw improvements in their blood sugar levels, however, the group that practiced IF experienced greater improvements. Participants in this group also reported better quality of life and greater satisfaction with their less restrictive diet.
The study authors do not fully explain the underlying mechanisms of IF on T2D, but point out that eating earlier in the day brings health benefits such as better 24-hour blood sugar control and better insulin sensitivity.
Another explanation could be that insulin levels are reduced during a fast and body fat stores begin to break down, which is beneficial for delaying or preventing T2D.
IF may be a viable alternative to calorie restriction for people with T2D. More research is of course needed to understand the long-term effects of IF on T2D and to determine the best protocols to follow.
In another study, researchers specifically observed the effects of IF on T2D. After 3 months, they found that IF reversed T2D in nearly half of the study’s participants. Other researchers in China evaluated the effects of 3 months of IF on T2D remission and found that 47.2% of participants no longer had diabetes after 3 months of IF.
Sources:
Nur Islami Mohd Fahmi Teng, Suzana Shahar, Nor Fadilah Rajab, Zahara Abdul Manaf, Mohamad Hanapi Johari & Wan Zurinah Wan Ngah (2013) Improvement of metabolic parameters in healthy older adult men following a fasting calorie restriction intervention, The Aging Male, 16:4, 177-183, DOI: 10.3109/13685538.2013.832191
Intermittent Fasting 101 — The Ultimate Beginner's Guide (healthline.com)
Intermittent Fasting: What is it, and how does it work? | Johns Hopkins Medicine